by Bocconi University
Legitimate prescriptions of opioids as painkillers are a contributing factor in long-term addiction to these substances. This is what Sarah Eichmeyer of Bocconi’s Department of Economics and Jonathan Zhang of McMaster University in Canada found and described in two recent papers, “Pathways into Opioid Dependence: Evidence from Practice Variation in Emergency Departments,” published on the American Economic Journal, and “Primary care providers’ influence on opioid use and its adverse consequences,” which appeared in the Journal of Public Economics.
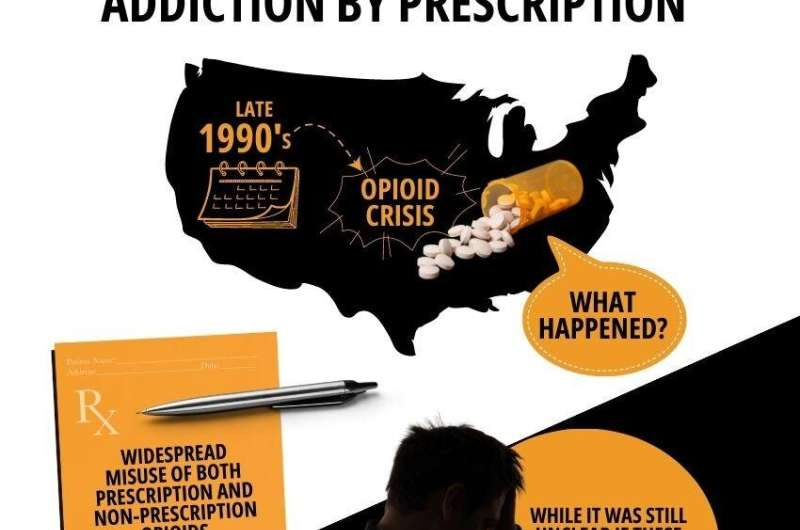
The so-called opioid crisis is a major concern in the United States. In short, since the late 1990’s certain pharmaceutical companies succeeded in reassuring the medical community that patients would not become addicted to opioid painkillers, and at the same time they started a very aggressive marketing effort on doctors who as a result began to prescribe them in huge quantities.
This led to widespread misuse of both prescription and non-prescription opioids before it became clear that these medications could indeed be highly addictive. But by then the situation had spiraled out of control and deaths from opioid overdose are now estimated to be in the hundreds of thousands for the last 20 years, with staggering social cost.
There is little hard evidence about the factors underlying opioid addiction. Looking at prescriptions is one logical way of approaching a scientifically sound analysis, but evaluating the actual effects of prescriptions on long-term addictions which can develop several years afterwards is very complex. Conducting clinical tests on vulnerable people is unethical, so a reliable dataset had to be found large enough for a statistically robust analysis.
The US Veterans Health Administration satisfied these conditions. Former members of the armed forces in the US have (mostly) free health care provided by dedicated facilities, and the authors were granted access to the medical records of about 2 million veterans, which is a large enough number for an accurate investigation.
The key fact here is that doctors’ inclination to prescribe opioids varies widely, even among doctors working in emergency rooms, which are the object of one of the two papers. The authors have proven not only that a causal relationship between prescriptions and addictions at a later stage exists, but they also measured its extent.
An opioid prescription originating from an emergency department (ED) visit increases the probability of long-term prescription opioid use, opioid addiction, and overdose mortality by 1.2, 0.34, and 0.075 percentage points, respectively. These numbers may look small, but they are not: they mean that out of every 1,400 people who walk out of an ED with an opioid prescription, one will eventually die of overdose.
“Our results highlight that long-term opioid use, misuse, and dependence can arise as a consequence of small variations in medical care received in a single medical encounter, at the emergency department. We find evidence that exposure to opioids via a prescription from the ED physician is the instance of medical care most likely to trigger these long-term effects,” Sarah Eichmeyer explains.
“At the same time, we do not find evidence for improved health—measured via improvements in pain—due to use of prescription opioids.”
